Can a few simple daily habits really help your body feel lighter and less swollen? If you’ve noticed tighter rings, snug clothes, or puffy wrists, those small clues can point to sluggish drainage in your system.
This short guide gives clear, friendly steps you can use right away. You’ll learn how breathing, movement, hydration, skin care, and gentle self-strokes support flow without special gear.
We’ll explain how this drainage differs from blood flow and why that matters for your overall health now. You’ll also see when hands-on massage or a drainage massage session may help—and when to skip techniques or call a clinician.
By the end, you’ll have a tiny daily routine to manage toxins and keep your body comfortable, plus simple signs to watch so you can act early.
Understanding Your Lymphatic System and Why It Matters for Health
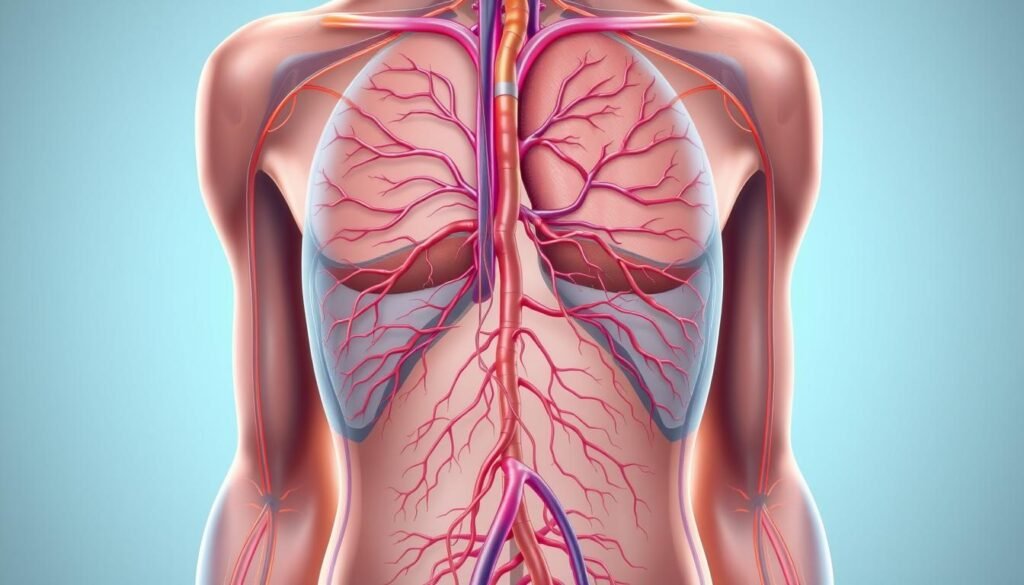
A quick map helps you see how fluid and larger particles leave tissues and find their way back into central circulation.
How it moves fluid, waste, and immune cells
You can think of the lymphatic system as your body’s cleanup and defense network.
Small vessels pick up extra fluid, bigger molecules, and waste that veins can’t return. That fluid—called lymph—travels one way toward central channels.
As lymph flows through nodes, immune cells screen for germs and support your immune system.
How this flow differs from blood circulation
Blood is pushed by the heart through arteries and back by veins. Lymph doesn’t have a central pump.
Instead, breathing, muscle movement, and vessel contractions nudge lymph forward. When transport slows, fluid and proteins can build up and cause swelling.
- Tip: Gentle movement and deep breaths help both systems work better.
- Note: Healthy flow is steady and quiet—your goal is to support it, not force it.
How to Tell If Your Lymphatic System Needs Support
You may notice everyday clues—snug rings or tight socks—that point to slowed fluid movement in a limb.

Common signs
Persistent swelling is the clearest sign. You might feel heaviness, aching, or a stretched sensation in an arm or leg.
Tighter clothes or jewelry on one side can be an early clue before visible change appears. Your skin may feel tight, warm, or uncomfortable over the area.
Linked conditions
Swelling and slower drainage often follow surgery, infection, trauma, or cancer treatment. Chronic venous insufficiency and lipedema can also put extra strain on the system.
- Snug rings, deep sock marks, or one sleeve fitting tighter.
- Heaviness or a sense of fullness that changes through the day.
- Persistent swelling in arms or legs that won’t resolve.
- Redness, warmth, or fever—seek medical care right away for possible infection.
If you’ve had nodes removed or recent surgery, watch one-sided changes closely. Early assessment helps you match the right support for the condition and can keep tissue healthy.
Lymphatic Detox: What It Means for You Today
Your body already moves larger particles and waste—your goal is to help that process run smoothly.
“Detox” here is not a radical cleanse. The lymphatic system collects fluid and particles veins can’t take back. Those materials travel toward central channels and then get processed or excreted by the kidneys and other organs.
When transport slows—after surgery, node removal, or radiation—protein-rich lymph can pool in tissue and increase infection risk. Gentle, steady support lowers that burden and helps your immune system and tissues work well.

- Breathing and movement nudge fluid toward central pathways.
- Hydration keeps fluid thin so drainage is easier.
- Light massage, done from center outward, complements daily habits.
Keep expectations realistic: improved energy, less heaviness, and smoother skin are common signs that your routine is helping. Aim for consistent, gentle actions rather than one-off extremes.
Five Natural Ways to Support Lymphatic Drainage at Home
With a few simple moves each day, you can help fluid clear from arms and legs more easily. Use brief, repeatable habits that pair breathing, movement, skin care, light self-massage, and posture to prime your system.

Deep diaphragmatic breathing
Start each morning with 3–5 minutes of belly breathing. Place a hand on your abdomen, inhale through your nose to expand the belly, then exhale slowly. This pressure change gently moves fluid toward central pathways and primes the chest and neck before working on a limb.
Gentle movement and exercise
Choose walking, cycling, or water aerobics to rhythmically contract muscles. Short, regular sessions nudge fluid forward and reduce buildup in your arms and legs without straining vessels.
Hydration and skin care
Drink water throughout the day and use mild cleansers plus fragrance-free moisturizer. Healthy skin lowers infection risk and preserves the barrier that helps the drainage process work well.
Self-manual techniques and timing
Learn light, directional strokes that move toward nearby nodes. Always begin at the neck and upper chest, spend 5–10 minutes per region, and keep strokes feather-light—stretch the skin slightly, don’t press into muscle.
Compression and posture habits
Wear well-fitted compression during active hours if recommended. Check your posture: stand and breathe every 45–60 minutes to avoid kinks where vessels and nodes sit.
Tip: Gentle, frequent care beats occasional intense sessions. Consider a professional lymphatic drainage massage to complement your home routine if heaviness persists.
Manual Lymphatic Drainage vs. Lymphatic Massage: What to Expect
A properly run session blends gentle, rhythmic strokes with a clear order so your body can move excess fluid more easily.
Evidence-based benefits for swelling, comfort, and tissue health
Drainage massage eases swelling from illness or medical treatment that clogs the lymphatic system. You may notice less heaviness, softer tissue, and clothes that fit better.
When used with compression, exercise, and skin care, manual lymphatic drainage is an effective part of Phase I treatment for lymphedema.
Inside a session: sequence from neck and central structures to the limb
Sessions run about 45 minutes. They start with deep breathing and gentle clearing at the neck and upper chest so central nodes and vessels are open.
After that, the therapist works outward—shoulder to hand for an arm—using light, directional strokes toward nearby nodes to encourage lymph fluid movement.
Risks and when it’s not right for you
Do not get drainage massage if you have a fever, active infection, or sudden redness and pain. Avoid direct manual stress over irradiated areas or known cancer sites.
- Share your medical history before treatment so the therapist can adapt techniques safely.
- Skip sessions during acute illness; seek clinical clearance first.
- If unsure, start with a consult to confirm this treatment fits your condition and goals.
Special Considerations After Cancer Treatment and Surgery
After surgery or radiation, your body may need extra, gentle care to keep fluid moving and tissues healthy.
Why this matters: Removal of lymph nodes or radiation can reduce transport capacity. That change lets protein-rich lymph collect in tissue and raise the risk of lymphedema over time.

Early monitoring and timely action
If you had breast cancer care, ask about early checks such as bioimpedance testing. These tools can spot subclinical changes before you notice fit differences in bras or sleeves.
Acting early with gentle strategies—breathing, careful self-strokes, and proper compression—often prevents progression to heavier, stiffer limbs.
Working with your care team
A focused plan may include a short course of manual lymphatic drainage, exercise guidance, skin care, and a fitted compression garment. Always avoid direct manual stress over irradiated areas or known cancer sites.
“Keep an eye on one-sided heaviness, fullness, or changes in clothing fit; report these signs promptly so your team can adapt care.”
- Watch for sudden redness, warmth, or fever — pause self-care and contact your clinician.
- Over the years your needs can change; schedule periodic checks to update garments and techniques.
When to Seek Professional Treatment—and When to Avoid Drainage
Know when to pause home care and seek professional help—small signs can mean urgent needs.
If swelling or discomfort is new, severe, or getting worse, get evaluated. A clinician can check for causes and recommend safe next steps or a tailored treatment plan.
Red flags that need immediate attention
- Fever, feeling acutely unwell, or rapidly spreading redness, warmth, or pain in an area—these suggest infection and need medical care first.
- Sudden one-sided swelling or new heavy fullness that won’t improve with rest and elevation.
- Signs of skin infection or red streaks—people with lymphedema are at higher risk of cellulitis and should call their clinician promptly.
When to avoid manual work over cancer or irradiated tissues
Do not apply direct manual pressure over a known cancer site, recent tumor area, or irradiated tissues. If you had breast cancer, removed nodes, or are in active oncology care, discuss safe alternatives with your team.
Tip: If any technique increases pain, numbness, or color changes, stop and seek guidance before continuing.
When in doubt, a short consult can protect healing areas and help you move safely toward relief.
Building Your At‑Home Maintenance Program
Turn clinical gains into lasting habits by pairing breathing, gentle movement, and light self-care each day. A brief, reliable routine keeps progress steady and makes support easy to stick with at home.
Daily routine: self-massage, breathing, gentle exercise, skin care
Start with 3 minutes of belly breathing to reset pressure in the chest.
Follow with a short mobility set and 5–10 minutes of light self-massage using gentle, directional strokes toward nearby nodes. These simple techniques prime the drainage system without strain.
Fit in gentle exercise most days—walking, cycling, or water work—to keep muscles pumping fluid from your legs and arms.
Skin care: keep skin clean and moisturized. Treat small cuts quickly and avoid harsh scrubs to reduce infection risk.
Choosing compression: daytime garments and nighttime options
Pick compression you will actually wear. A comfortable daytime garment should support activity without pinching.
For sleep, ask about multi-layer wrapping or specific night garments if your clinician recommends them. Proper fit feels supportive, not painful.
Tracking swelling, heaviness, and fit over time
- Note a favorite ring’s fit and sock marks weekly.
- Write how sleeves or shoe fit change and any new swelling or heaviness.
- Scale techniques back if skin becomes sore or irritated, and reassess with your care team when patterns shift.
Tip: an occasional lymphatic drainage massage tune-up during travel or stressful periods helps you stay ahead of heaviness.
Store your garments, moisturizer, and a water bottle where you see them. Small habits lead to steady wins — like easier shoe fit or less end-of-day swelling — and they tell you the program is working.
Conclusion
Small, steady actions can keep fluid moving and make your arms and legs feel lighter.
You now understand how your lymphatic system partners with blood flow to clear waste quietly. Focus on easy daily habits: breathing, gentle movement, skin care, light self-strokes, and fitted compression.
If you need extra help, consider a short series of drainage massage or massage sessions. Safety matters: pause for red flags and check with your clinician before starting hands-on work.
Pick two habits to start today, add a third next week, and reassess in a month. Share your plan with the people who support you and revisit it over the years as your needs change.
, With steady, gentle care you can help your body feel lighter, move easier, and protect your long-term health.
FAQ
What does the lymphatic system do and why should I care?
The lymphatic system moves fluid, waste, and immune cells through vessels and nodes to support tissue health and fight infection. It works differently from blood circulation by relying on breathing, movement, and muscle contractions rather than a central pump. Keeping it healthy helps reduce swelling, lower infection risk, and support recovery after surgery or cancer treatment.
How can I tell if your lymphatic system needs support?
Watch for swelling, a heavy or tight feeling in limbs, rings or clothes that suddenly fit differently, and skin discomfort. These signs can point to fluid buildup, early lymphedema, or venous issues. If you notice sudden redness, heat, or pain, seek medical care right away.
What does “detox” mean for lymph and tissues?
In this context, “detox” means helping your body move excess fluid and cellular waste from tissues into circulation so immune cells can process and remove it. It’s not a single cure-all—supportive habits like breathing, movement, hydration, and gentle massage aid natural clearance.
What simple practices support drainage at home?
Five effective steps are deep diaphragmatic breathing, regular gentle movement or exercise, staying well hydrated and caring for your skin, using light self-massage strokes directed toward nearby nodes, and mindful compression and posture to help vessel flow.
How do deep breaths help fluid flow?
Diaphragmatic breathing creates pressure shifts in the chest and abdomen that pull fluid toward central lymphatic channels. Practicing slow, full breaths several times daily boosts central drainage and reduces peripheral pooling.
Are self-manual techniques safe and how do I do them?
Yes, gentle surface strokes that follow the proper direction toward major nodes are safe for most people. Use light pressure—enough to stretch the skin but not compress tissue—working from limbs toward the neck and trunk. Stop if you feel pain, increased swelling, or redness.
What’s the difference between manual lymphatic drainage and a regular massage?
Manual lymphatic drainage uses very light, rhythmic strokes focused on directing fluid toward nodes and central channels. Traditional massage often uses deeper pressure aimed at muscles. For swelling or postsurgical care, manual techniques are usually preferred.
When is professional treatment recommended?
Seek a certified therapist if you have persistent or worsening swelling, a history of lymph node removal or radiation, suspected lymphedema, or uncertain symptoms. Professionals can provide assessment, tailored treatment, and compression fitting.
Are there situations when drainage should be avoided?
Yes. Avoid manual drainage with an active infection, fever, blood clots, uncontrolled heart failure, or rapidly spreading redness and pain. Also use caution over recent cancer sites or irradiated tissue—get clearance from your oncology or surgical team first.
How does compression help and how do I choose a garment?
Compression supports vessel function, reduces fluid buildup, and maintains treatment gains. Daytime garments come in different classes and fits; a trained fitter or clinician can recommend the right pressure and style based on your needs and daily activities.
What special care do people need after breast cancer surgery?
After node removal or radiation, monitor for early signs of swelling, practice gentle range-of-motion and breathing exercises, protect skin from cuts or infection, and consult your care team before any massage over the surgical area. Early referral to therapy can prevent progression.
How do I build a simple daily maintenance routine?
Combine daily diaphragmatic breathing, short sessions of gentle movement (walking, yoga, or light strength work), brief self-massage toward nodes, good skin hygiene and hydration, and wearing recommended compression during active hours. Track fit of clothing and limb measurements to spot changes early.
Can exercise make swelling worse?
Properly chosen gentle exercise usually reduces swelling by pumping fluid through muscles. Avoid heavy resistance or high-impact workouts that strain tissues until a clinician approves. Start slow and monitor for increased heaviness or tightness.
How soon should I see a professional if I suspect lymphedema?
See a certified therapist or your healthcare provider as soon as you notice persistent swelling, asymmetry, skin changes, or reduced range of motion. Early assessment and intervention improve outcomes and lower long-term risk.