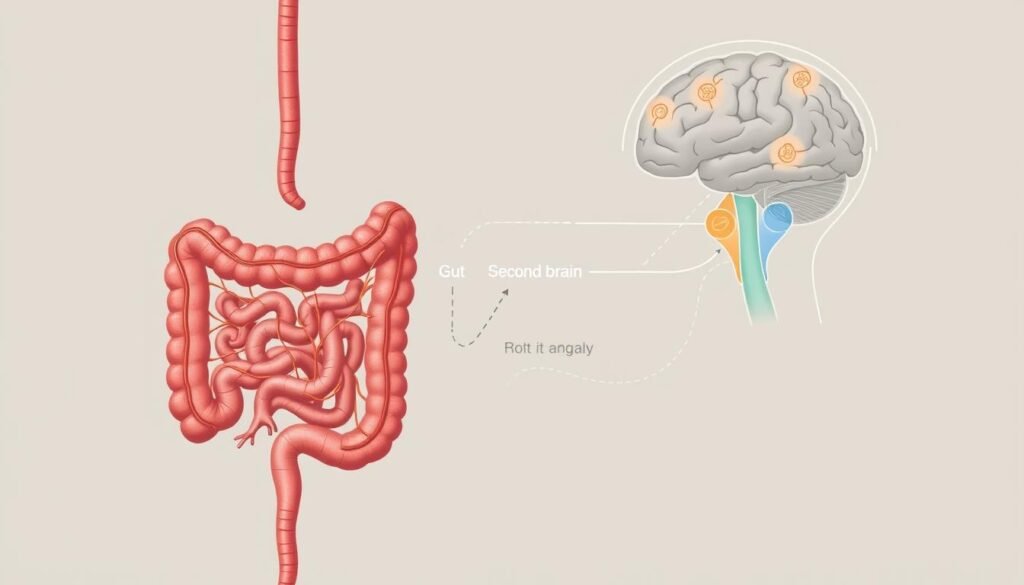
Did you know your gut has its own nervous system? Often called the “second brain,” it contains over 100 million nerve cells. These cells constantly communicate with your actual brain, influencing mood, stress, and even anxiety.
Research from Johns Hopkins reveals a surprising link. Gut irritation can send signals that trigger depression or anxiety. Nearly 40% of people with digestive issues also experience mood changes. For women, this connection may be even stronger.
Why? Serotonin, the “feel-good” chemical, is mostly made in the gut. When your digestive health suffers, so can your mental well-being. Could improving your gut ease stress and boost happiness? Let’s explore how this powerful link shapes women’s health.
Understanding the Gut-Brain Connection
Your gut isn’t just digesting food—it’s shaping your emotions. This happens through a complex network of neurons, chemicals, and nerves that constantly chat with your brain. Let’s break down the key players.
Your “Second Brain”: The Enteric Nervous System
The enteric nervous system (ENS) is your gut’s own command center. With over 500 million neurons, it controls digestion from start to finish—without needing your brain’s input. Swallowing, breaking down food, and even elimination are all managed here.
When the ENS gets irritated, it sends distress signals to your brain. This can trigger mood swings or anxiety. Research links ENS dysfunction to IBS and mental health disorders.
Key Players: Vagus Nerve and Gut Microbiome
The vagus nerve acts like a superhighway, carrying 80% of gut-brain traffic. It’s a two-way street: your gut tells your brain when something’s wrong, and your brain responds. This is why stress can upset your stomach—and vice versa.
Your gut microbiome—trillions of bacteria—also plays a role. These microbes produce serotonin, GABA, and dopamine. Stanford studies show diverse gut bacteria boost dopamine, lifting mood. In fact, stimulating the vagus nerve is now an FDA-approved depression treatment.
How the Gut-Brain Connection Works
Your body has a hidden communication network linking digestion and emotions. This system relies on two key players: the vagus nerve and your gut microbiome. Together, they send signals that affect everything from mood to motivation.
The Vagus Nerve: Your Gut-Brain Superhighway
Think of the vagus nerve as a two-way radio between your gut and brain. It handles 80% of their communication, regulating digestion without conscious input. Harvard research found damage to this nerve may lower Parkinson’s risk by 40%.
When your gut is irritated, the vagus nerve fires distress signals. This can trigger anxiety or brain fog. Stanford scientists linked long COVID cognitive issues to low serotonin from gut inflammation.
Gut Microbes and Mood: The Role of Bacteria
Your gut microbiome—home to trillions of bacteria—acts like a tiny pharmacy. It produces chemicals that influence your mind:
- Bifidobacterium and Lactobacillus boost dopamine by 25%.
- Microbiome transplants reduced anxiety in mice studies.
- Stanford found microbial metabolites even affect exercise motivation.
Feed these helpful bacteria with fiber-rich foods. A diverse gut microbiome supports mental clarity and emotional balance.
The Gut-Brain Link to Mental Health
Mental health struggles might start in your gut, not just your mind. Research shows chronic stress can alter gut bacteria, sparking inflammation that worsens anxiety or depression. Here’s how this hidden link works—and what you can do about it.
Stress, Inflammation, and Mental Health
When you’re stressed, cortisol spikes. This hormone can weaken your gut lining, causing “leaky gut.” Toxins then enter your bloodstream, triggering inflammation linked to mood disorders.
Stanford researchers found fermented foods (like yogurt) reduce inflammation markers by 15%. This suggests calming your gut may ease mental health symptoms.
- Cortisol increases pro-inflammatory bacteria by 300%.
- 64% of IBS patients also meet criteria for anxiety disorders.
- Johns Hopkins found antidepressants soothe gut nerve activity.
Serotonin: More Than Just a Brain Chemical
Your gut produces 90% of your body’s serotonin. This “feel-good” chemical regulates sleep, appetite, and emotional resilience. Low levels are tied to depression and insomnia.
Animal studies show microbiome transplants reduce anxiety. Diversity matters—a rich mix of gut bacteria may lower PTSD risk.
Want to boost serotonin naturally? Try fiber-rich foods like oats or bananas. They feed good bacteria that support your mood.
Why Women Are Especially Affected
Women’s bodies have a unique relationship between hormones and digestion that impacts mental well-being. Monthly cycles, pregnancy, and menopause all trigger changes in gut health that can amplify mood swings or anxiety.
Hormones, Gut Health, and Mood Swings
Estrogen receptors line your intestinal tract. When levels drop before your period, digestion slows by 30%. This can cause bloating and discomfort that worsens PMS symptoms.
Progesterone increases intestinal permeability during ovulation. This “leaky gut” effect allows toxins to enter your bloodstream, potentially triggering inflammation-linked mood disorders.
IBS and Mental Health in Women
Women comprise 65-70% of IBS diagnoses. NIH studies show female patients have 2.5x higher anxiety risk than men with the same conditions.
Serotonin plays a dual role—regulating both menstrual cycles and gut function. Low levels may explain why women are twice as likely to develop depression after an IBS diagnosis.
| Hormone | Effect on Digestion | Mental Health Impact |
|---|---|---|
| Estrogen | Speeds motility (high phase) | Reduces pain sensitivity |
| Progesterone | Slows motility, increases permeability | Linked to PMDD mood swings |
| Cortisol | Triggers inflammation | Worsens anxiety |
Key takeaways for women:
- Track digestive changes throughout your cycle
- Fiber-rich foods help balance estrogen effects
- Probiotics may ease hormone-related bloating
Signs Your Gut Is Affecting Your Mental Health
Ever notice how your mood shifts with stomach troubles? Your digestive issues might be more than just physical—they could be influencing your emotions. Research shows 72% of people with depression also report GI problems, suggesting a strong link between gut health and mental well-being.

Digestive Issues and Mood Changes
Specific symptoms often pair with emotional shifts. For example, bloating can trigger irritability, while constipation may cause brain fog. A Johns Hopkins study found that CBT for IBS reduced diarrhea and anxiety by 50%.
Chronic stress worsens this cycle. It alters your gut microbiome, reducing diversity by 40%. This imbalance fuels inflammation, which Stanford links to mood disorders.
Food Cravings and Emotional Eating
Your cravings might signal microbiome distress. Sugar cravings correlate with low bacterial diversity, as bacteria thrive on sugary diets. This sparks dopamine-seeking behavior, making you crave more junk food.
Nighttime cravings? Blame melatonin. Your gut produces 50% of this sleep hormone. Imbalances disrupt sleep and increase hunger hormones like ghrelin, leaving you “hangry.”
| Symptom | Emotional Impact | Fix |
|---|---|---|
| Bloating | Irritability | Probiotics + peppermint tea |
| Sugar cravings | Low energy | Fiber-rich snacks |
| Constipation | Brain fog | Hydration + magnesium |
Key takeaway: Track how your gut reacts to stress or certain foods. Small changes, like adding fiber, can rebalance both digestion and mood.
How to Support Your Gut-Brain Health
Small daily habits can reshape how your gut and brain communicate. Research shows simple changes to your diet and lifestyle improve this vital connection. Here are science-backed ways to nurture both digestion and emotional balance.

Probiotics and Prebiotics: Feeding the Good Bacteria
Specific probiotics target stress resilience. Bifidobacterium longum reduces anxiety scores by 18% in six weeks. Pair them with prebiotics like garlic or apples to fuel beneficial microbes.
Try Stanford’s 4-Week Fermented Food Protocol:
- 1 serving daily of yogurt, kefir, or sauerkraut
- Gradually increase to 6 servings weekly
- Diversity matters—rotate different fermented foods
Mind-Body Therapies for Gut-Brain Harmony
Therapy isn’t just talk—it heals your gut too. Johns Hopkins found CBT reduces IBS hospitalizations by 35%. Physical exercise like yoga improves symptoms by 60% in 12 weeks.
Try these vagus nerve toning techniques:
- Humming activates gut motility
- Cold showers boost nerve signaling
- Deep belly breathing reduces stress
Diet and Lifestyle Changes That Help
Turmeric and ginger repair gut lining while reducing inflammation. Magnesium-rich foods (spinach, almonds) ease both constipation and muscle tension.
Simple ways to start today:
- Swap processed snacks for fiber-rich berries
- Drink peppermint tea for bloating relief
- Take 10-minute walks after meals
Conclusion
Taking care of your gut could be the key to better mental well-being. Start with three steps: test your microbiome, manage stress with techniques like deep breathing, and prioritize fiber-rich foods.
Stanford’s research on Parkinson’s and gut bacteria shows promise, while Johns Hopkins offers telehealth for personalized gut-brain health support. Small changes—like swapping processed snacks for berries—add up.
Your health journey begins at the dinner plate. Try one new way to nourish your gut today, and notice the shift in your mood and energy.
FAQ
What is the gut-brain connection?
It’s the two-way communication between your digestive system and your brain. Your gut sends signals to your brain, and your brain influences digestion, mood, and overall health.
How does the vagus nerve affect mental health?
The vagus nerve acts like a superhighway, carrying signals between your gut and brain. A healthy vagus nerve helps regulate stress, anxiety, and inflammation.
Can gut bacteria really impact my mood?
Yes! Your gut microbiome produces chemicals like serotonin, which affects happiness and well-being. An imbalance in bacteria may contribute to mood swings or depression.
Why are women more affected by gut-brain issues?
Hormonal changes, stress sensitivity, and conditions like IBS are more common in women. These factors can disrupt gut health and worsen mental health symptoms.
What are signs my gut is affecting my mental health?
Frequent bloating, food cravings, or mood shifts after eating may indicate a gut-brain imbalance. Stress-related digestive issues are also a red flag.
How can I improve my gut-brain health?
Eating probiotic-rich foods, managing stress, and staying active support a healthy gut. Mind-body practices like yoga can also strengthen this connection.
Does serotonin come from the gut?
About 90% of serotonin is made in your digestive system. A healthy gut helps maintain balanced serotonin levels, which influence mood and sleep.
Can gut health help with anxiety?
Yes! Reducing inflammation and supporting good bacteria may ease anxiety. Foods like yogurt, fiber-rich veggies, and fermented items can help.



