Do you ever wonder why your gut feels different in your 40s and 50s—and what small swaps could change that?
Many people face gas, constipation, or irregularity as hormones and lifestyle shift. About 15% of people in Western countries live with IBS, a sign that gut sensitivity rises with age.
This guide gives a friendly, science-backed path to the best foods for digestion in midlife so you can feel more comfortable day to day. You’ll learn simple swaps, fiber and fermented options, and practical tips that help your system stay balanced.
Try easy breakfast upgrades and smarter snacks, and use meal timing and hydration to amplify results. If symptoms persist, tracking patterns and talking with a clinician helps protect your long-term health.
For a deeper nutrition plan tailored to women over 35, check this nutrition blueprint.
Why midlife digestion changes and how the right foods can help
As you move through midlife, changes in hormones and muscle tone often shift how your digestive system works. This can slow transit and make you notice new sensitivity or symptoms like gas, heartburn, or irregularity.
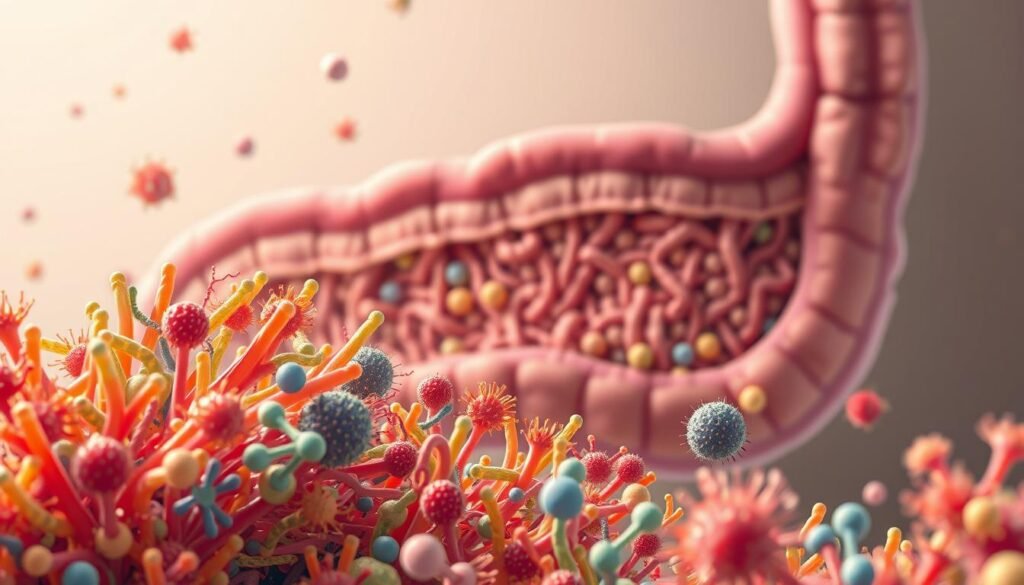
Fiber matters. When fiber is fermented by gut bacteria, it produces short-chain fatty acids that support the cells lining the colon. Those cells help immune function—about 70% of immune cells live there—so what you eat affects overall health.
Practical swaps help. Choose steady fiber, fluids, and fermented options to feed beneficial microbes and improve how your body breaks down and absorbs nutrients. Easier-to-digest meals can also support a healthy weight by keeping you satisfied without overload.
“Small, consistent steps in nutrition often beat occasional big changes.”
- Focus on plant-forward plates and lean proteins.
- Swap refined grains for whole ones; add a fermented side.
- If new or worsening symptoms persist, see a clinician to rule out underlying issues.
The best foods for digestion to ease bloating and support a healthy gut
Small swaps at meals can ease bloating and help your gut work more smoothly through midlife. Focus on steady sources of fiber and live cultures to keep your colon functioning well.
Whole grains and leafy greens
Choose whole grains instead of white bread and refined pasta to reach at least 25 grams of fiber a day. When gut bacteria ferment fiber, they make short-chain fatty acids that support colon cell function.
Low-fructose fruits and avocado
Pick low-fructose fruits — berries, citrus, and bananas — to reduce gas and feed good microbes. Add avocado in modest portions for extra fiber and potassium without a big fructose load.
Fermented options, prunes, and plant protein
Work in kefir, kimchi, sauerkraut, or miso to introduce beneficial bacteria into your plate. Keep prunes handy to ease constipation and support regular bowel movements.
- Oats and beans feed your microbiome and provide steady energy.
- Choose lean protein like poultry, fish, tofu over fatty meat.
- Drink water, milk, or herbal tea so fiber can work properly each day.
Foods and habits to limit for a healthier digestive system
Certain meals and habits can quietly worsen how your stomach feels—knowing which to limit helps you stay comfortable.
High-fat choices and red meat can speed colon contractions and cause post-meal cramps. The higher fat content in some red meat also shifts bacteria that may raise cardiovascular risk. Cut portions and pick lean cuts to protect gut and overall health.

Refined grains that shortchange fiber
White bread and standard pasta lower your daily fiber. That shortfall can slow transit and worsen bloating. Swap whole-grain versions to keep your system moving and reduce uncomfortable symptoms.
Caffeine, fizzy drinks, and spicy triggers
Caffeinated or carbonated drinks increase stomach acid and may lead to heartburn and bloating. Spicy sauces, onions, and garlic often provoke symptoms in sensitive people—scale them back before busy days.
- Grill, bake, or air-fry to lower added fat without losing flavor.
- Pair richer meals with extra vegetables to balance fat and fiber.
- Monitor consumption and keep a simple note of what triggers your gut; personal patterns matter.
If symptoms persist despite these changes, check with your healthcare provider to rule out other causes and refine your plan.
Daily fiber and fluid: simple upgrades that curb constipation
A simple change to how you drink and eat fiber often cuts constipation and steadies your system. Small, consistent moves can give your digestive system the support it needs without a big reset. Aim for variety so your gut gets different types of fuel that help overall health.
Hit about 25–30 grams of fiber a day from varied sources
Most people fall short. Build intake from oats, beans, wholemeal bread, brown rice, fruit, vegetables, and seeds so you reach roughly 25–30 g per day. Increase intake slowly over a few weeks to reduce extra gas and let your body adapt.
Pair fiber with steady hydration so it can work properly
Fiber absorbs water like a sponge. Drinking fluids—especially water—softens stool and helps move waste through the digestive tract. A glass of water with each meal is a simple, practical habit.

- Daily target: Aim for 25–30 g and mix sources—oats, beans, whole grains, fruit, and vegetables.
- Gradual increase: Add fiber slowly and sip water to reduce discomfort and protect bowel function.
- Easy swaps: Try chia in breakfast, brown rice at lunch, and a bean side at dinner.
- On the go: Pack a high-fiber snack and a refillable bottle to keep habits steady each day.
“Small, steady changes in your diet and fluids often give the biggest wins in gut health.”
If constipation continues despite these tips, check in with your clinician to review medication, testing, or tailored changes to protect long-term health.
When your gut is sensitive: IBS-friendly strategies that work
When your gut feels unusually reactive, practical steps can cut flare-ups and help you eat with more confidence.
Irritable bowel syndrome affects about 15% of people in Western countries. If you suspect bowel syndrome, a structured plan helps you learn what triggers gas and bloating without guessing.
Try a structured low-FODMAP approach if symptoms persist
Work with a clinician or registered dietitian on a short elimination phase. Remove high-FODMAP items, then reintroduce specific items slowly to spot which foods like certain fruits, dairy, or wheat-based products cause symptoms.
Consider a probiotic trial taken daily for at least four weeks to see if it eases your digestive system discomfort. Track changes so you can report progress at follow-ups.
- Keep meals simple during flares: baked seabass, rice, cooked greens, and ripe bananas calm the gut.
- Use gentle cooking and smaller, more frequent portions to reduce sensitivity.
- Rebuild variety slowly so your microbiome and gut bacteria stay nourished while you identify triggers.
“The goal is a flexible plan you can live with, not long-term restriction.”
If symptoms affect sleep, work, or social life, bring those concerns to your provider. Combine nutrition with stress management, movement, and steady sleep to protect overall health as you troubleshoot.
Conclusion
,Small, reliable habits around fiber, fluids, and fermented items help your digestive system stay steady over time.
Center your plate on plants, whole grains, lean protein, and lower-fructose fruits most days. Add kefir, kimchi, sauerkraut, or miso to bring live bacteria into meals and support a healthy gut.
Keep fiber steady and pair it with water to reduce constipation and gas. Limit high fat meals and red meat to fewer occasions to lower risk and ease stomach discomfort.
Make simple swaps each week—whole-grain toast, yogurt with berries, a bean side—to broaden nutrients and keep your bowel comfortable. If symptoms persist, check in with your clinician to refine your diet and protect long-term health.
FAQ
Why does your digestion change in midlife and how can food help?
As you enter midlife, your metabolism and hormone levels shift, your gut motility can slow, and your microbiome composition often changes. Choosing fiber-rich whole grains, leafy greens, fermented items like kefir or kimchi, lean proteins, and staying well hydrated helps support regular bowel function, feed beneficial bacteria, and reduce bloating.
Which whole grains should you pick instead of white bread to support colon function?
Opt for oats, brown rice, barley, and whole-wheat bread or pasta that list “whole grain” first on the label. These choices provide soluble and insoluble fiber that ease stool passage, feed gut bacteria, and supply sustained energy without the quick sugar spike of refined grains.
How do leafy greens like spinach and kale help your gut and microbiome?
Leafy greens deliver fiber, magnesium, and microbiome-friendly sugars that encourage beneficial bacteria growth and improve bowel regularity. You can add them to smoothies, salads, or lightly sauté them for easier digestion if you’re sensitive to raw vegetables.
What low-fructose fruits are gentler on your stomach and still good for gut bacteria?
Berries (strawberries, blueberries), citrus (oranges, grapefruit), and bananas are relatively low in fructose and provide fiber, vitamin C, and antioxidants. They support healthy bowel movements without triggering excess gas for many people.
Is avocado a good choice if you have digestive concerns?
Yes—avocado offers soluble fiber, potassium, and healthy fats that are usually gentle on the gut. Keep portions moderate because the high fat content can bother people with fat sensitivity or reflux.
How do fermented foods like kimchi and sauerkraut help gut bacteria?
Fermented foods contain live cultures that can boost levels of beneficial microbes in your gut. Regular, moderate servings of kefir, miso, yogurt with active cultures, kimchi, or sauerkraut may improve digestion, reduce bloating, and support immune health.
Can prunes really relieve constipation and how should you use them?
Prunes are high in fiber and contain sorbitol, a natural laxative. A small daily portion—about 3 to 4 prunes—can soften stools and improve regularity. Start with a modest amount and increase if needed to avoid gas or cramping.
Why are oats, beans, and other plant fibers important for your microbiome?
These foods provide prebiotic fibers that feed beneficial bacteria, producing short-chain fatty acids that nourish the colon lining and reduce inflammation. Gradually increase servings to let your gut adapt and combine them with fluids to prevent constipation.
Should you choose lean protein over high-fat red meat for better gut comfort?
Yes. Poultry, fish, and plant proteins like tofu digest more easily and tend to cause fewer symptoms than high-fat red meats, which can slow gastric emptying and trigger discomfort or colon contractions in sensitive people.
What hydration choices support fiber and overall gut function?
Plain water is best, but milk and herbal teas also hydrate and help fiber form soft, moveable stools. Aim to sip throughout the day rather than drink large amounts only at meals.
Which snacks give vitamin C without too much fructose?
Citrus segments, strawberries, and blueberries are great options. They provide vitamin C and antioxidants while keeping fructose moderate, which helps reduce gas for those with sensitivity.
What high-fat foods and red meats should you limit to reduce digestive issues?
Cut back on fatty cuts of beef and processed red meats, fried items, and heavy cream sauces. These can provoke reflux, slow digestion, and cause cramping or loose stools in some people.
Why avoid refined grains like white bread and pasta if you want better gut health?
Refined grains lack fiber and micronutrients, which can lead to harder stools, less fuel for your microbiome, and greater blood sugar swings. Swap them for whole-grain alternatives to improve bowel regularity and nutrient intake.
How do caffeine and fizzy drinks affect bloating and heartburn?
Caffeine can relax the lower esophageal sphincter and trigger heartburn, while carbonated beverages introduce gas that stretches the stomach and increases belching or bloating. Limit them if you notice symptoms.
Should you avoid spicy foods, onions, and garlic entirely if you have sensitivity?
Not necessarily—many people can enjoy small amounts without issue. If you experience heartburn, gas, or IBS symptoms after these foods, reduce portion sizes or try cooked versions, which are often gentler than raw.
How much fiber should you aim to eat daily to curb constipation?
Aim for about 25–30 grams of fiber per day from varied sources: whole grains, fruits, vegetables, legumes, nuts, and seeds. Increase fiber gradually and pair it with adequate fluids to let it work effectively.
Why must you pair fiber with steady hydration?
Fiber absorbs water to form a soft, bulky stool that moves smoothly through the colon. Without enough fluid, fiber can harden stool and worsen constipation, so sip water throughout the day.
What is a low-FODMAP approach and when should you try it?
A low-FODMAP plan limits fermentable carbs that often trigger IBS symptoms like bloating, gas, and pain. Try it if you have persistent symptoms despite general diet changes, ideally under guidance from a registered dietitian to ensure balanced nutrition.
When should you see a clinician about persistent gut symptoms?
See your clinician if you have unexplained weight loss, blood in stool, severe pain, persistent constipation or diarrhea, or symptoms that don’t improve with diet and lifestyle changes. These signs may indicate a condition needing medical evaluation and targeted care.



