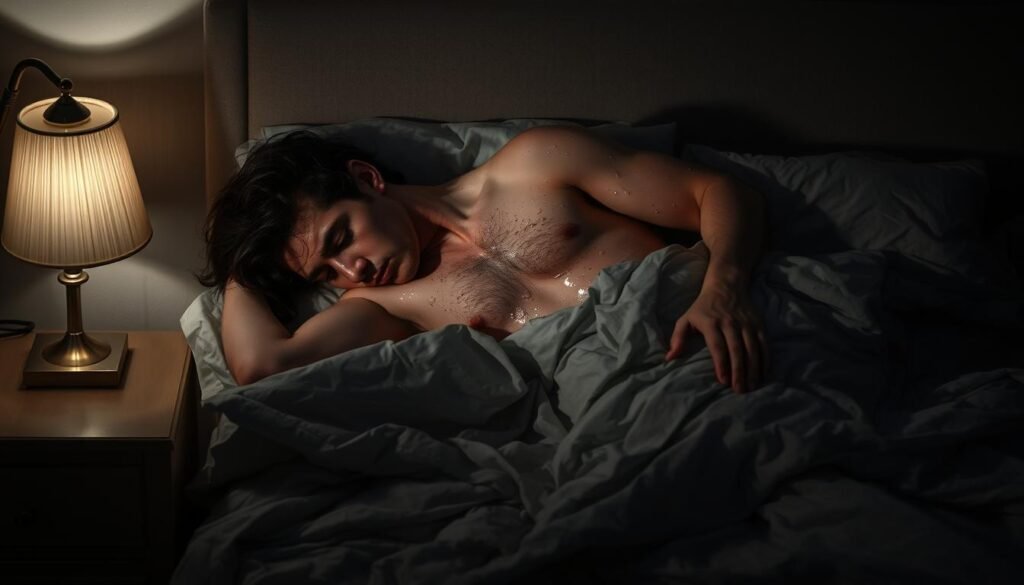
Have you ever woken up drenched and wondered what your body is trying to tell you? That sudden heat, soaked sheets, and ruined sleep can feel alarming. You deserve clear answers and simple fixes.
This guide gives you a friendly roadmap to understand why this happens after age 35, how hormone changes can make your hypothalamus misread your temperature, and what to try tonight to sleep through the rest of the night.
You’ll learn the common causes—from menopause and thyroid issues to medications and infections—and when symptoms point to a need for medical help. You’ll also get seven practical fixes like cooling your room, switching to breathable bedding, and cutting evening alcohol or spicy foods.
For a deeper look at nutrition and midlife health that can ease hot flashes and other symptoms, see this nutrition blueprint for women over 35. Start here and take back restful, cool sleep tonight.
What Night Sweats Are and Why They Disrupt Your Sleep
True night sweats soak your sleepwear even when the room feels cool, signaling an internal reset of your body’s thermostat.
How your thermostat and thermoneutral zone work at night
Your thermoneutral zone is the narrow temperature band where your body feels comfortable. During sleep that band can shift, so small internal changes trigger sweating as a cooling response.
Sleep changes your thresholds. Your body lowers the point where it starts to sweat or shiver. That makes you more sensitive to hormonal shifts, infections, or certain drugs.
Night sweat vs. a hot bedroom: key differences that matter
Check the room first: if the AC or fan is on, bedding is light, and airflow is good, but your sheets are soaked, the cause is internal. That helps separate a true episode from simple room heat.
- You may notice related symptoms like restless sleep, insomnia, or anxious awakenings.
- Tracking timing, meals, or alcohol use helps you and your clinician find the most likely causes.
- Lowering bedding heat and improving airflow still helps, even when the root cause is internal.
Night Sweats in Women: The Most Common Causes After 35
Many triggers can make you wake hot and drenched; knowing the likely culprits helps you target fixes fast.

Hormonal shifts and reproductive cycles
Perimenopause and menopause are the top drivers after age 35. Declining estrogen and progesterone narrow your temperature comfort zone and spark hot flashes and night sweats. Perimenopause often starts in your 40s; full menopause follows after 12 months without a period (average age 51).
PMS or PMDD can cause episodes just before your cycle. Pregnancy can raise night sweating, often peaking near week 30 and again shortly after delivery. Premature ovarian insufficiency may cause menopausal symptoms before 40 and deserves prompt medical review.
Common medical conditions
- Thyroid disease (especially hyperthyroidism) — look for palpitations and tremor.
- Diabetes and autonomic changes that alter temperature control.
- Hyperhidrosis and obstructive sleep apnea, which have distinct daytime signs like daytime sleepiness.
Infections, cancer, meds, and stress
Fever-producing infections—flu, COVID-19, tuberculosis, or bacterial endocarditis—can cause night sweats as your body cools. Certain cancers (leukemia, lymphoma) and many cancer therapies also lead to drenching episodes and weight loss; new, severe sweats merit urgent evaluation.
Medications (antidepressants, steroids, and some diabetes and blood pressure drugs), alcohol, and substances can all trigger symptoms. Anxiety and stress sensitize sweat glands and worsen sleep, making episodes more frequent.
“Track timing, meds, and any weight or fever changes to help your clinician find the cause.”
Key Symptoms and Red Flags You Shouldn’t Ignore
Not all episodes are equal—certain signs mean it’s time to see a doctor.

If you wake drenched while the room feels cool, pay attention to other symptoms. New or unexplained weight loss, a persistent fever, chest or localized pain, or a cough that won’t go away are clear red flags.
When sweating points to fever, weight loss, cough, or pain
These signs can signal infections or serious disease. Infections like flu, COVID‑19, or tuberculosis often cause nighttime temperature spikes followed by intense sweating. Certain cancers such as non‑Hodgkin lymphoma or leukemia can also present this way.
Patterns, severity, and timing that warrant a doctor’s visit
- Drenching episodes that repeat for days or wake you from deep sleep.
- Sweating with swollen nodes, ongoing fatigue, pallor, or steady loss of appetite or weight.
- Daytime symptoms—breathlessness, palpitations, insomnia, or worsening anxiety and stress—that accompany episodes.
Tip: Track how often episodes occur, how soaked your bedding gets, and any triggers. Clear details help your clinician pick targeted tests.
How Doctors Evaluate Night Sweats
A concise home log gives your clinician the clues they need to find the root cause. Bring simple records and a short symptom history so your visit is focused and efficient.

- One- to two-week log noting when episodes occur, how soaked bedding gets, and room temperature.
- Foods or drinks before bed, plus alcohol, caffeine, and nicotine use.
- A complete list of prescriptions, OTC drugs, and supplements.
- Sleep details: bedtime, awakenings, snoring, gasping, or daytime sleepiness.
Typical clinical workup you can expect:
- A focused history on onset, frequency, and triggers, plus a hands-on exam of temperature, blood pressure, thyroid size, lymph nodes, and lung/heart sounds.
- Blood tests to check blood counts, thyroid function, glucose, and markers of infection or inflammation.
- Targeted testing when indicated — infectious disease screening, imaging, or a sleep study for suspected obstructive sleep apnea.
Tip: Your clinician may adjust or replace medicines that provoke sweating and will screen for hyperhidrosis if no clear cause appears.
Seven Fixes to Cool Down Fast and Sleep Better Tonight
Try simple, proven steps you can do this evening to lower temperature and sleep more soundly.

Optimize your bedroom climate and bedding
Set the bedroom cool and run a fan or AC for steady airflow. Use lightweight, breathable bedding layers you can peel back if you get warm.
Tame evening triggers
Avoid alcohol, caffeine, spicy meals, and late workouts. These raise internal heat and can cause night sweats.
Adopt a cooling wind-down
Sip chilled water, take a lukewarm shower, and try brief breathing or relaxation to lower nervous system arousal.
Dress smart and time activity
Wear moisture‑wicking sleepwear and choose natural fibers. Finish exercise and heavy meals 2–3 hours before bed to protect sleep.
Tip: Keep spare pajamas and a light towel near the bed so you can reset quickly and return to sleep.
- Support metabolic health with regular day activity to help manage weight.
- Plan a medication review with your clinician if episodes started after a new drug; never stop meds on your own.
Targeted Treatments Based on Cause
Treatment choices depend on the underlying cause, so your plan should be specific and practical.
Menopause-related hot flashes: hormone and nonhormonal options
If menopause is the driver, clinicians may offer menopausal hormone therapy when appropriate. Nonhormonal meds and lifestyle tools also cut hot flashes and improve sleep.
Addressing sleep apnea, thyroid imbalance, and hyperhidrosis
If sleep apnea causes episodes, CPAP or other airway therapies often reduce night sweating and boost daytime alertness.
Treating hyperthyroidism or restoring normal thyroid levels usually lowers sweating and palpitations as well.
For excess sweating unrelated to other issues, prescription topicals, oral meds, or botulinum toxin injections can help control symptoms.
Treating infections and understanding when antibiotics or antivirals help
Infections need targeted therapy: antibiotics for bacterial disease, antivirals when indicated, and specific regimens for tuberculosis. Symptoms ease as the illness is treated.
Behavioral health care for anxiety and stress-linked sweating
Mindfulness, brief cognitive behavioral techniques, and stress reduction lower sympathetic arousal that fuels sweating. Combine these with cooling bedding and sleep-hygiene changes for faster relief.
Tip: Expect some approaches to work within days, while apnea care or hormone adjustments may take weeks to fully improve night sweats.
Your Ongoing Plan: Prevention, Tracking, and Better Sleep
Build a simple nightly routine that tracks what you eat, the room climate, and any symptoms so you can spot patterns fast.
Make a tiny tracker you’ll actually keep
One line per morning is enough. Note episodes, room temperature, any spicy food or alcohol, and where you were in your cycle.
Use tags like “wine,” “late workout,” or “spicy dinner” so patterns stand out. Record weight trends and medication changes to share with your clinician.
Set your bedroom up for consistent success
Keep steady airflow with a fan or AC and use breathable bedding and moisture‑wicking pajamas. Layer bedding so you can peel back without waking fully.
Set a cut‑off for heavy meals, caffeine, and late exercise. Schedule regular daytime movement to support sleep and reduce body heat spikes at night.
- Short wind‑down: 10 minutes of breathing or gentle stretching to lower stress and anxiety before bed.
- Hydration tip: Sip chilled water earlier in the evening and keep a cool bottle near the bedside.
- Share your log: Bring it to appointments to speed diagnosis and treatment decisions.
Tip: Consistent tracking plus a cool, well‑ventilated bedroom gives you the best chance to reduce episodes and improve sleep fast.
Conclusion
, You’re not alone. Many people over 35 experience night sweats, and clear steps help you cool down and sleep better tonight.
Know the causes—hormone changes, medications, infections, sleep apnea, or thyroid issues—and watch for red flags like unexplained weight loss, fever, pain, or a persistent cough. Use the seven fixes: cool the room, choose breathable bedding, avoid evening triggers, hydrate, and reduce stress. Track episodes so you can spot patterns.
Next steps: Try the simple changes now and see your clinician if worrisome symptoms appear. With small daily habits and targeted treatment, your nights may also become calmer and more restorative.
FAQ
What exactly causes heavy night sweats after age 35?
Hormone changes around perimenopause and menopause are common triggers, but other causes include thyroid problems, diabetes, infections like influenza or COVID-19, certain cancers, medication side effects, alcohol or spicy late-night meals, and anxiety. Lifestyle and bedroom temperature also influence how much you perspire while sleeping.
How can I tell if it’s a hot room or a medical problem?
If symptoms ease after lowering room temperature, using a fan, or switching to breathable bedding, it’s likely environmental. Seek medical care when sweating is severe, happens with fever, unexplained weight loss, persistent cough, night pain, or if it disrupts sleep despite a cool bedroom—those are red flags for underlying disease.
Could my prescription or supplements be causing this?
Yes. Antidepressants, some diabetes drugs, hormone therapies, steroids, and certain supplements can raise night sweating. Review your medications with your clinician and never stop a prescribed drug without medical advice. Adjusting dose or switching treatments often reduces symptoms.
What simple steps can I try tonight to reduce episodes?
Cool your room to 60–67°F, use moisture-wicking sleepwear and lightweight sheets, keep a fan for airflow, avoid late alcohol, caffeine, and spicy meals, hydrate earlier in the evening, and practice a calming pre-sleep routine to cut stress-driven sweating.
When should I see a doctor about these episodes?
Make an appointment if you have fever, unexplained weight loss, night pain, chronic cough, severe sleep disruption, or if sweating starts suddenly and intensely. Also see your provider if lifestyle changes don’t help or if you suspect medication or a hormonal issue.
What tests might a clinician order to find the cause?
Expect a focused history and physical exam, blood tests for thyroid function, glucose, complete blood count, and inflammatory markers. Depending on findings, your clinician may order chest imaging, hormone panels, sleep testing for apnea, or targeted infection testing.
Are there effective medical treatments for menopause-related hot flashes and sweating?
Yes. Hormone therapy often works well for many people and nonhormonal options like low-dose SSRIs, SNRIs, gabapentin, or clonidine can help. Topical and device-based treatments exist for focal excess sweating. Discuss risks and benefits with your clinician.
How does anxiety cause night perspiration, and what helps?
Anxiety activates your sympathetic nervous system, raising temperature and sweat. Cognitive behavioral therapy, stress-reduction techniques, regular exercise (timed earlier in the day), and, when appropriate, medications can lower anxiety-related episodes.
Can infections or cancer show up first as heavy nighttime sweating?
Some infections like tuberculosis or severe viral illnesses and certain cancers (for example, lymphoma) can present with drenching nocturnal perspiration. These usually come with other signs—fever, weight loss, cough, or swollen lymph nodes—so report those to your clinician promptly.
What lifestyle changes help long-term control and prevention?
Maintain a healthy weight, limit evening alcohol and caffeine, eat earlier and avoid spicy late meals, optimize bedroom airflow and bedding, track symptoms and triggers, and address sleep apnea or metabolic issues to reduce recurring episodes over time.